Revision Rhinoplasty
Conveniently located to serve the areas of Englewood and Denver, CO

Revision Rhinoplasty
Revision rhinoplasty refers to surgery on the nose after it has previously been operated on. Some surgeons will refer to any repeat surgery including ones they have previously done as a revision. Others will differentiate calling revision surgery only ones they have previously done, while secondary rhinoplasty would be ones performed by another surgeon. The number of prior rhinoplasties can vary from one to more than ten, each with varying complexity and approaches. Regardless of terminology, this type of rhinoplasty can be very challenging and complicated.
If you are unhappy following your initial nose reshaping surgery, schedule a visit with our Denverteam by calling (303) 839-7980 or inquiring with our contact form to see if revision rhinoplasty is right for you. At Colorado Facial Plastic Surgery, our surgeries can include minor changes to enhance aesthetics or more comprehensive reconstruction to reshape the nose.
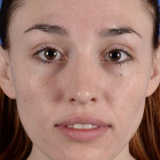
Before and After Photos
Contents
About Revision Rhinoplasty
Revision rhinoplasty is a specialized surgical procedure aimed at correcting nasal deformities, improving the appearance of the nose, enhancing overall facial harmony, and addressing breathing difficulties resulting from prior nasal surgeries. The procedure is typically performed via an open approach. This is where incisions are made inside as well as along the columella. This allows for complete exposure of the underlying cartilages and bony framework. Improved breathing and/or cosmetic appearance are the goals of revision rhinoplasty.
Candidates (1)(2)(3)

There are multiple different reasons for seeking a revision rhinoplasty. We have listed common reasons below. This list, although comprehensive, may not fit your exact situation. Please also review the “Candidates” section of our Primary Rhinoplasty page to learn more; there may be an overlap in candidates between both primary and revision rhinoplasty.
Over-Resected Nose
The over-resected nose in revision rhinoplasty refers to overdoing the concept of reduction as discussed previously. Taking away too much from the nose is not a good thing. Some patients desire very petite noses while in their youth. To achieve this result, some surgeons will simply cut away the areas needing reduction without respect for long-term outcomes. As the patient ages, the skin continues to contract; without proper support in the form of cartilage grafts, the nose can appear too small, pinched, or unsightly. Furthermore, the resected structures, like skin and cartilage, may make breathing very difficult.
Common areas that are over-resected are the bridge and tip. The “swoop” on profile used to be popular but is now associated with an overly-operated appearance. When the tip is too small, it may appear to be isolated or like a “ball” at the end of the nose. To improve this, your surgeon will place grafts to raise the bridge. Widening the tip to create better harmony with the remainder of the nose may be necessary.
To correct these deformities, grafting is needed. The normal cartilage of the nose may be too thin or damaged which defeats their function. Grafting with cartilage helps to restore form and thus function. By putting in the grafts, the nose in some areas may appear wider. This is intentional to restore breathing to the nose. The widening is very subtle if done well but is a tradeoff. In areas where thickened skin is needed, soft tissue such as temporalis fascia provides excellent augmentation.
Rebuilding the nose after too much is taken can be difficult. Your surgeon may have to use a large source of cartilage and place the graft to make the nose appear wider.
Pinched Nose
Often related to the over-resected nose, the pinched nose occurs when the structure is too narrow. The tip and nasal bones are the most common areas for this to occur. The desire to create a small, “cute” nose can lead to this problem. Our approach involves using structure to rebuild the nose.
A refined tip has a gentle flow from the bridge toward the base and nostrils. When the tip is pinched, the nose can appear like a “ball” on the end of the nose and disconnected from the rest. To improve this, the surgeon must deconstruct the tip and place cartilage grafts. They will need to remove scar tissue and sutures placed from a previous surgery and reconstruct the nose into an anatomic form. They may place soft tissue grafts over the top of the tip structure to further cover any imperfections previously created.
The surgeon will move nasal bones inward to help create narrowness of the upper third on front view. Osteotomies are the bone cuts that allow surgeons to perform these maneuvers. The nasal bones are delicate and not overly thick when compared to other facial bones. Too aggressive mobilization inward of the nasal bones can result in a pinched appearance. The flow from nasal bones toward the tip then becomes disjointed. To correct this problem, the nasal bones need to be out-fractured back toward a more normal position. This isn’t always possible especially if the bones are comminuted (broken into many, small pieces) from improper technique. If that’s the case, the surgeon can provide camouflage in the form of soft tissue to improve symmetry within reason.
The pinched nose is an unsightly complication from prior rhinoplasty. During the consultation, we will emphasize the dangers of creating too narrow of a nose to avoid this problem.
Upturned Nose
The upturned nose refers to a nose that appears to be too rotated. As a result, there is often a “piggy” look where too much of the inside of the nostril is seen in front view. The tendency during rhinoplasty is to rotate the tip without consideration for how little movements can create large degrees of change. The ideal nasolabial angle for males is 90-95 degrees, while in females it is 95-105 degrees. To follow the angle closely during surgery, we employ a tool called a goniometer which helps measure the angle to within 5 degrees of accuracy.
When the nose is too rotated, scar tissue can develop making counterrotation extremely difficult. A large, caudal septal extension graft is used to help set the tip into a new position. The amount of movement that can be achieved is related to the pliability of the skin. If the skin is tight pre-operatively, the amount of counter rotation is much more limited. A way to improve this is with stretching exercises and sometimes hyperbaric oxygen. Stretching involves pulling the skin outward and down to create biological creep of the tissues. Patients should hold the tip in the new position for 20 seconds, 15-20 times per day for sometimes several months before surgery. This creates flexibility of the skin and can allow for better outcomes during surgery.
Relatedly, with upward rotation of the nose, we can see alar retraction or arched nostrils. This can contribute to seeing more of the inside of the nose. Composite grafts from the ear and lateral crural strut placement with repositioning of the native crus both help to lower the nostril margin. Doing so can recreate better harmony with the counter rotation of the tip. Fixing the upturned nose can create a much-improved frontal and profile view. Expectations regarding the amount of counter rotation need to be clear based on the patient’s unique anatomy and the surgeon’s skill set.
Post-Traumatic Deformity
A post-traumatic deformity is a result of trauma to the nose which changes the shape and/or function. Crooked or deviated noses are one of the most common deformities we see. This can affect the appearance of the nose as well as its function. Sometimes, there is tissue loss from an injury such as a dog bite or skin cancer. Drugs such as cocaine or autoimmune diseases like Wegener’s Granulomatosis (also known as Granulomatosis with Polyangiitis) can also be culprits. Fixing these types of deformities can require multiple stages.
The crooked nose can be caused by blunt trauma, particularly to the nasal bones, which shifts the entire structure. Osteotomies and septoplasty are often required to fix the nose in a more midline position. Perfect symmetry post-surgery is very difficult to achieve, which is why we review patients’ preoperative expectations. We advise patients to avoid wearing glasses or participating in too strenuous activity post-operatively. It is very important to not shift the nose.
Dog bites and skin cancer can result in large tissue defects. The skin, cartilage, and mucosa (inner lining of the nose) can all be involved. The surgeon may need to replace the cartilage framework with tissue and obtain tissue from the septum or ear. The mucosa may require flaps of adjacent mucosa which are rotated into position. Finally, the skin is where art meets function. The surgeon may have to remove full-thickness skin grafts from one spot (usually in front of the ear) and place them into a defect. The skin will integrate with the surrounding tissues over time and is a relatively fast, easy procedure for small defects.
The surgeon may have to create local tissue flaps from creating designs of adjacent skin that are incised and rotated to fill the defect. They must craft the flaps to be the perfect size to allow for good function and camouflage. At times, the surgeon may require multiple stages to attain full skin coverage in cases in which they create axial or pedicle flaps from the forehead or cheek. The reason for this is to establish blood flow and slowly create the ideal, anatomic contour. Also, despite best efforts, the cosmesis may not be ideal. That’s where we employ CO2 laser and Intense Pulsed Light to help revise the tissues and scarring with great success.
Drugs such as cocaine and autoimmune diseases like Wegener’s can destroy cartilage, particularly in the septum. Cocaine creates perforations within the septum as does Wegener’s. This can lead to a lack of support to the nose creating a saddle nose deformity. This requires substantial reconstruction using rib cartilage. It is critical to ensure that all drug usage has permanently stopped. Also, in the case of Wegener’s Granulomatosis, a doctor must confirm the diagnosis and control the symptoms using medicines under the guidance of a rheumatologist. Trauma is a unique opportunity to restore form and function to the nose. If possible, the surgeon can repair the nose in one stage. Sometimes, though, it is in the patient’s best interest to stage procedures over weeks to months for the best outcome.
Cleft Lip-Nose
The cleft lip-nose is a congenital deformity that occurs during the formation of the nose and lip in utero. The lip can have a small or substantial portion missing that requires correction due to feeding needs. The nose with its relation close to the upper lip may be affected as well. With this condition, the nasal tip pulls to the side opposite of the cleft as does the septum. The nostril on the side of the cleft is horizontally oriented and pulled posteriorly, and the tip is under-projected and wide. There are varying degrees of deformity though the aforementioned description is considered classic for cleft nose.
Correction of this deformity often requires a multi-stage approach via multiple surgeries over months to years. A multidisciplinary team is often required for younger children; the nasal repair must occur over time as the facial skeleton and nose continue to develop toward maturity. Breathing concerns are corrected using septoplasty. The surgeon must utilize grafting and an open approach for the most meticulous correction. The nostril often requires substantial reorientation in tandem with unique grafts and local flaps.
Although the surgeon will have to complete the surgery in multiple stages, the results cosmetically and functionally can be quite good. We even see patients who had their initial procedures as children and wait decades to undergo further refinement. This does not preclude a rhinoplasty and it can be helpful as goals are often very realistic.

Personal Consultation
The initial consultation is critical to understand not only patient expectations but also to gain information regarding prior surgeries. Although some surgeons review old medical and operative reports, this is not always needed, useful, or available. Many patients will be able to reiterate the original reason for surgery, the timeframes, and the postoperative course. Some patients even provide pre-operative photos which can be helpful. Physical examination assists with visualizing old scars, functional deficits if any, and undesired changes. The clues from this examination will give your surgeon insight into how the prior surgeries might have been performed (i.e. scar on columella would indicate an open approach).
Photography is crucial to be able to objectively evaluate the structure of the nose. Your surgeon may morph the images and discuss these possible outcomes with you. Morphing involves changing the shape of the nose using software to create a desired result, although it is not a guarantee of outcome. Your surgeon will take photos of your nose from multiple angles, in good lighting. They will then fully analyze and discuss your areas of interest. certain asymmetries may become more apparent to you. A large portion of our consultation is spent reviewing the patient’s photos.
With knowledge of the prior procedures, current photographs, and desired goals, the surgeon can formulate a plan concurrently with the patient. You can take the first steps today by calling our Denver practice at (303) 839-7980 or filling out our online form.
Preparation
A preoperative visit will typically occur 1 to 2 weeks before your surgery. During this time, you will meet with our nurse who will review – in detail – all day-of-surgery and post-operative instructions. This will include reviewing medications to take before and/or after surgery, phone numbers for issues post-operatively, and wound care. The patient will also meet with the surgeon to finalize all plans for the procedure. This may include reviewing goals for the operation and morphed photos.
Procedure
Distinguished from primary rhinoplasty by its heightened complexity, revision rhinoplasty demands an elevated level of expertise and finesse due to the presence of scar tissue and the altered nasal anatomy resulting from previous surgical interventions. The procedure occurs at a hospital or surgery center under general anesthesia. Depending on the extent of work being performed, the procedure will last anywhere from 3 to 7 hours. You will be discharged home with a follow-up in the clinic within 1 week.
Recovery
The first follow-up visit occurs within 1 week after the procedure. At that visit, your surgeon will remove the cast, tape, splints, and sutures. They will clean and evaluate all wounds. They will re-emphasize the importance of wound care- especially antibiotic soaks- and schedule your next follow-up visits. Aside from walking, you should restrict vigorous exercise for 3 to 4 weeks post-surgery. Pain is often mild for the first few days and manageable with medications. If your surgeon harvested rib cartilage, you should engage in deep breathing and walking to assist with recovery. A low-salt diet with plenty of fluids will help to reduce swelling. You should not blow your nose until cleared by your surgeon.
Results (4)
The nose will appear quite swollen upon cast removal, but this is in no way representative of the final outcome. In revision rhinoplasty, healing takes longer since the tissues have been previously operated upon. The profile view often “shows” the result faster than the front view. Think of it this way: you look at yourself in the mirror every day and will not appreciate subtle change as compared with the profile view which you do not see as often. Most of the healing will be complete after 12 months, though each patient can vary, and some may need longer. We cannot stress enough the importance of follow-up visits to ensure the best possible result and patience during the healing process. If any asymmetries occur, we often recommend waiting 10 to 12 months to ensure swelling has gone down and settling has been maximized before proceeding.
Cost of Revision Rhinoplasty in Denver
Revision rhinoplasty pricing can vary depending on the complexity of the case. Surgeon’s fees can range anywhere from $7500 to over $15,000. Please remember that these numbers do not include the cost of the facility and anesthesia. At Colorado Facial Plastic Surgery, we strive to make procedures as affordable as possible with financing options like Prosper and CareCredit. To get started with a consultation today, call (303) 839-7980 or use our contact form, and a member of our team will promptly help you find a date and time that aligns with your schedule.
References
- Toriumi DM. New Concepts in Nasal Tip Contouring. Archives of Facial Plastic Surgery. 2006;8(3):136-185. doi:https://doi.org/10.1001/archfaci.8.3.156
- Toriumi DM. Nasal Tip Contouring: Anatomic Basis for Management. Facial Plastic Surgery & Aesthetic Medicine. 2020;22(1):10-24. doi:https://doi.org/10.1089/fpsam.2019.29006.tor
- Toriumi DM. Structure approach in rhinoplasty. Facial Plastic Surgery Clinics of North America. 2005;13(1):93-113. doi:https://doi.org/10.1016/j.fsc.2004.07.004
- Toriumi DM, Kowalczyk DM, Cristel RT, et al. Evaluation of Postoperative Infection Rates in 3084 Rhinoplasty Cases Using Antibiotic Soaks and/or Irrigations. Facial Plastic Surgery & Aesthetic Medicine. 2021;23(5):368-374. doi:https://doi.org/10.1089/fpsam.2020.0465